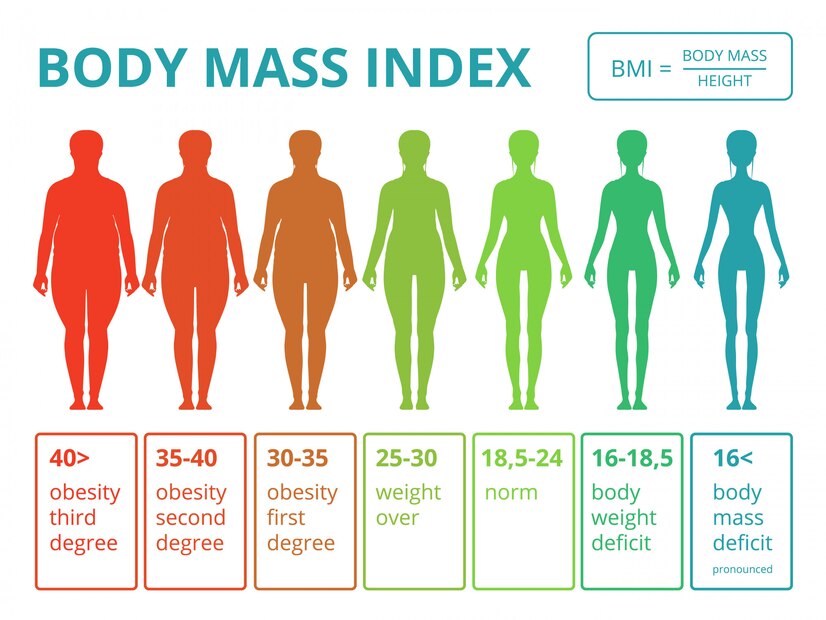
¿Es Hora de Abandonar el Índice de Masa Corporal (IMC)?
DOI:
https://doi.org/10.18041/2665-427X/ijeph.1.3877Palabras clave:
IMC, Exactitud, Validez, Rata de Probabilidad Máxima, Distribución anormalResumen
Introducción: El estudio fue realizado con la finalidad de estimar la exactitud en la medición del estado nutricional de las personas utilizando la nueva fórmula del Índice de Masa Corporal (IMC), teniendo como parámetro de comparación el IMC tradicional.
Métodos: El análisis de exactitud fue realizado mediante la estimación de la sensibilidad, especificidad, valor predictivo positivo y negativo, los índices de Youden y Kappa, además de la razón de máxima verosimilitud y la curva ROC.
Resultados: Aunque la nueva fórmula IMC arrojó resultados similares a la fórmula tradicional en la mayoría
de los indicadores examinados. Ambas fórmulas presentan una distribución muy sesgada a la derecha, siendo mayor en la nueva fórmula comparada con la tradicional. Los resultados fueron mayores en la nueva fórmula, siendo 5.91 y 4.81 en el grupo de sobrepeso, y 30.9 and 30.3, en el grupo obeso.
Conclusión: Si bien los resultados encontrados apuntan a que la nueva fórmula se comporta de forma similar a la fórmula original y, por tanto, podrían ser utilizadas en forma intercambiable. Los hallazgos señalan que ambas fórmulas presentan una amplia dispersión hacia la derecha, sesgo que afecta la validez en la medición del sobrepeso y obesidad, resultado que no permite ser recomendadas.
Descargas
Referencias
1. Quetelet A. Recherches sur le poids de l’homme aux différens ages. Nouv Mem l’Academie R Des Sci B-Lett Bruxelles. 1832; 7: 1‐43.
2. Keys A, Karvonen N, Kimura N, Taylor HL. Indices of relative weight and obesity. J Chronic Dis. 1972; 25:329–3. Int J Epidemiol, 2014; doi:10.1093/ije/dyu058.
3. Garrow JS, Webster J. Quetelet’s Index (W/H2) as a Measure of Fatness. Internat J Obesity. 1985; 9:147–153.
4. Vandevijvere S, Chow CC, Hall KD, Umalia E, Swinburna BA. Increased food energy supply as a major driver of the obesity epidemic: a global analysis. Bull World Health Organ. 2015; 93:446–456.
5. Kleinert S, Horton R. Rethinking and reframing obesity. Lancet. 2015; 385: 2326-2328.
6. OMS. Informe sobre la situación mundial de las enfermedades no transmisibles. 2010. Resumen de orientación. Ginebra: OMS; 2011.
7. Thorpe KE, Florence CS, Howard DH, Joski P. The impact of obesity on rising medical spending. Healtj. Aff (Millwood). 2004; Suppl Web Exclusives: W4-480–6,
8. House of Commons Health Committee. Obesity. Third Report of Session 2003–04. Volume I Report, together with formal minutes. London; 2004.
9. Allender S, Rayner M. The burden of overweight and obesity related ill health in the UK,” Obes Rev. 8(5): 467–73, 2007.
10. Dee A, Kearns K, O’Neill C, Sharp L, Staines A, O’Dwyer V, et al. The direct and indirect costs of both overweight and obesity: a systematic review. BMC Res Notes. 2014; 7: 242.
11. Dobbs R, Sawers C, Thompson F, Manyika J, Woetzel J, Child P, et al. Overcoming obesity: an initial economic assessment. A discussion paper. McKinsey Global Institute; 2014. Available from: https://www.mckinsey.com/~/media/McKinsey/Business%20Functions/Economic%20Studies%20TEMP/Our%20Insights/How%20the%20world%20could%20better%20fight%20obesity/MGI_Overcoming_obesity_Full_report.ashx (accessed July 29,2018).
12. Trefethen N. BMI is flawed. Professor of numerical analysis. University of Oxford. Letter to the Economist. January 5, 2013.
13. Fletcher RW, Fletcher SW. Clinical Epidemiology: The essential. Four edition. Lippincott Williams & Wilkins; 2005.
14. Gordis L. Epidemiologia. 3er edición. Elsevier: España. Madrid; 2005.
15. Oliveira AG. Biostatistics Decoded. John Wiley & Sons; 2013.
16. Statistical Analysis Software. SAS/STAT Software. Avalaible from: https://www.sas.com/en_us/software/stat.html.
17. IBM SPSS. Statistics software, version 24.0. SPSS Incorporated IBM Company. Chicago, Illinois. United States.
18. Flegal KM, Kit BK, Orpana H, Graubard BI. Association of allcause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013; 309: 71–82.
19. Yi SW, Ohrr H, Shin SA, Yi JJ. Sex-age-specific association of body mass index with all-cause mortality among 12, 8 million Korean adults: a prospective cohort study. Int J Epidemiol. 2015; 44: 1696–705.
20. Smith GD, Ebrahim S. Mendelian randomization: can genetic epidemiology contribute to understanding environmental determinants of disease? Int J Epidemiol. 2003; 32: 1–22.
21. Zajacova A, Ailshire J. Body mass trajectories and mortality among older adults: a joint growth mixture-discrete-time survival analysis. Gerontologist. 2014; 54: 221–31.
22. Twig G, Yaniv G, Levine H, Leiba A, Goldberger N, Derazne E, et al. Body-mass index in 23 million adolescents and cardiovascular death in adulthood. N Engl J Med. 2016; 374: 2430–40.
23. Berrigan D, Troiano RP, Graubard BI. BMI and mortality: the limits of epidemiological evidence. Lancet. 2016; 388: 734-6.
Descargas
Publicado
Versiones
- 2018-05-30 (4)
- 2021-06-21 (3)
- 2021-06-21 (2)
- 2018-11-07 (1)
Número
Sección
Licencia
Derechos de autor 2018 Revista Interdisciplinaria de Epidemiología y Salud Pública

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial-SinDerivadas 4.0.